Varicose veins of the lower extremities are a problem that plagues more than 60% of the world's population. The term "varicose" from the Latin "varix" is interpreted as "dilation". Therefore, the definition of the pathological state-dilation of the venous cavities of the lower extremities and pelvic organs, which significantly impairs the blood flow in the blood vessels, thereby worsening the patient's general condition. In the following material, we will consider the causes of varicose veins, the possible complications of the disease, and the main ways to deal with the pathology.
Causes and risk factors: everyone is susceptible to this influence
important:If varicose veins are more than young people under 25, then the gender distribution here occurs at 50: 50. In other words, boys and girls have the same condition. At a more mature age, women are more likely to have varicose veins due to pregnancy and significant changes in age-related hormone levels.
If we consider varicose veins from the inside, then anatomically, the dilation of the venous lumen is due to the malfunction of the venous valve that regulates blood flow. A malfunctioning valve does not close completely with each heartbeat. As a result, blood from the heart convulsively moves to the lower limbs due to gravity.
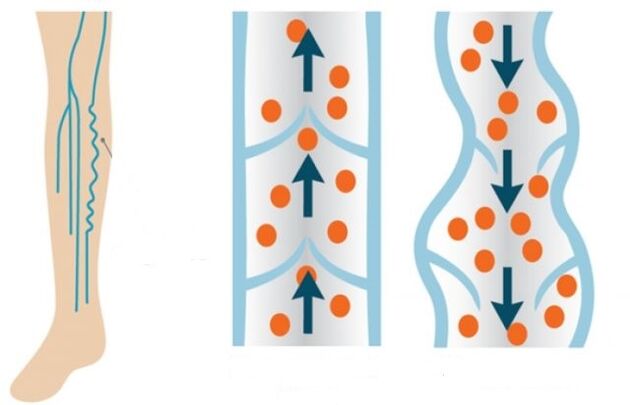
Under normal circumstances, the valve should close and allow blood to flow to the legs in fractions. However, unfortunately, because the valve system functions equally poorly, the blood flow enters the legs more intensively, while in the opposite direction, its movement is less intense. Over time, the blood-filled leg veins lose their elasticity and stretch.
The main predisposing factors for the development of vascular pathology are:
- Genetic component (the disease can be transmitted through female or male lines in the family);
- Overweight;
- Postpone pregnancy
- Passive lifestyle
- Excessive physical activity;
- Smoking and drinking;
- hormone imbalance.
Male problem
If we consider the causes of varicose veins, depending on the gender of the patient, then they are somewhat different in men and women. To be more precise, each representative of a different gender is easy to develop certain habits, and these habits will sooner or later cause vascular lesions in the lower extremities. Therefore, for men, the risk factors are:
- Strength training for lifting weights from a squat position;
- Overweight and obesity;
- Unbalanced diet, leading to frequent constipation;
- Pathological processes of the kidneys (tumors of various etiologies);
- Inguinal hernia;
- Sedentary work
- Smoking and drinking.
important:Men are characterized not only by the development of varicocele in the lower extremities, but also by the development of varicocele. This pathology is called varicocele. This condition is hereditary, that is, it is completely hereditary in nature, and it cannot be prevented even by strengthening preventive measures. Only 2-4% of men suffer from varicocele. The pathological cause is the asymmetry of the anatomical position and structure of the male reproductive organs.
Because men suffer from false shyness or do not have time to see a specialist at the beginning of the disease, varicose veins are more difficult for them than women.
Women's varicose veins have their own rules
For women, varicose veins are more "familiar" than men. More than 80% of women suffer from vascular disease in the legs. In addition, the risk group includes fairer genders who prefer this lifestyle or experience the following:
- Wearing tight-fitting high heels;
- Working sedentary or standing;
- Genetic predisposition
- Changes in hormone levels during pregnancy or when suffering from autoimmune diseases;
- Wearing tight underwear and jeans;
- smokes;
- Low proportion of fruits and vegetables in the diet (continuous diet and hunger);
- Like to tan (go to the solarium often or stay in direct sunlight);
- Rapid weight gain;
- Low liquidity.
Pregnancy is where "dogs are buried"
Even if the manifestations of varicose veins are not initially observed in women, the cause and treatment can only be determined and prescribed by a phlebologist, but in 30% of cases, it becomes obvious during pregnancy. Here, the main flaw is the growing fetus and the uterus that comes with it, which strongly squeezes the pelvic organs. As a result, blood circulation in the lower body is significantly impaired. It is difficult for blood to flow upward from the legs. This effect on the deep veins of the legs causes the blood vessels to be actively stretched in width and length.
In addition to the growth of the uterine organs and the pressure on the blood vessels of the pelvic organs, varicose veins in pregnant women also develop under the influence of the following factors:
- Increased coagulation function. Therefore, nature ensures that women do not lose a lot of blood during childbirth. Thick blood is more difficult to pass through veins.
- The increase in the level of the hormone progesterone causes the uterine muscles and blood vessels to relax, so as the fetus grows, it can increase freely and without tension. But at the same time, the remaining blood vessel walls also relax. The veins become less elastic, and the thick blood stretches the blood vessel walls that have been weakened by progesterone.
- Increased blood pressure provides a better supply of oxygen to the fetus. Therefore, the body will try to quickly drive thick blood through the loose blood vessels. For this reason, its volume in the legs increases.
- As the belly grows, pregnant women have difficulty in mobility. This leads to stagnation of blood in the legs and pelvic organs.
Complications of varicose veins
If varicose veins are not treated and paid attention to, patients may experience very serious complications over time, and may even require comprehensive surgical intervention. In the worst case, the patient may amputate the diseased limb. Below we will consider the most common and dangerous complications of varicose veins.
Chronic venous insufficiency
As this complication develops, the venous valve will actively malfunction. In addition, the pathological process is divided into four stages:
- zero. After a hard day, the patient felt slight swelling and infrequent soreness in his legs.
- First. On the surface of the skin, a network of veins that dilate blood vessels can be seen.
- second. Swollen veins with blood clots and nodules are clearly visible. Inflamed veins, itching, and ulcers will turn red in the skin area.
- third. Nutritional ulcers on the legs and inflammation of the veins.
important:Signs of chronic venous insufficiency include leg itching, soreness, burning sensation during prolonged sitting, swelling, and night cramps.
Superficial vein thrombophlebitis
In this case, the patient has a tendency to form blood clots. The clot actively blocks the venous cavity, making it difficult for blood to flow. In most cases, blood clots and clots are located in the blood vessels of the lower third of the thigh or the upper third of the leg. The symptoms of venous thrombophlebitis are:
- Redness of the skin on the legs where the blood clot is formed;
- Leg pain
- Palpation-venous induration.
important:People with thrombophlebitis must wear compression stockings. The compression formula should be chosen by an expert-a vascular surgeon or a phlebologist.
Trophic ulcer
This complication has already manifested in the later stages of venous insufficiency. First, the patient's vascular permeability increases. A white seal with a varnish-like surface is formed on the skin surface. Ulcers form under it. At the slightest injury to the inflamed area, the ulcer is opened and the exudate begins to separate. Wounds with exudate can be infected secondary, leading to a purulent inflammatory process.
important:In this case, the wound needs to be completely healed first, and then a full surgical intervention is performed to remove the affected blood vessel.
Pulmonary embolism
An equally dangerous complication in which a blood clot separates from an inflamed vein and moves to the pulmonary artery. This artery directly participates in the blood flow in the small circle of tissue and affects the right ventricle of the heart. If the diameter of the shed thrombus is smaller than the artery lumen, the clot moves to the branch of the pulmonary artery, causing pulmonary edema or infarction. In this case, the patient will feel significant chest pain. Symptoms such as wet cough and mixed blood, increased body temperature, and weakness may also occur. If the diameter of the clot is equal to the diameter of the pulmonary artery lumen, the patient will instantly block and die.
The following conditions can trigger blood clot detachment:
- Undergo a surgical operation;
- Oncology;
- heart failure;
- Long-term bed rest.
Conservative treatment and surgical treatment
Varicose veins can be treated conservatively and surgically, depending on the pathological stage and the patient's condition. Conservative treatment requires intravenous injection of drugs. On the surface, a horse chestnut-based gel and venom ointment are used. It should be understood that conservative treatment only works in the initial stages of varicose veins.
As an additional measure for conservative treatment of varicose veins, physical activity (walking) and the wearing of compression stockings are shown.
Minimally invasive and surgical treatment methods
If the process of varicose veins and venous insufficiency is far away, then they adopt minimally invasive or comprehensive surgical intervention to improve the patient's condition. Minimally invasive intervention methods include:
- Sclerotherapy. In this case, a fine insulin needle is used to inject a special hardening drug into the lumen of the patient's varicose veins. The injected substance first causes inflammation and then hardens the diseased vein. The lumen of the diseased blood vessel just grew out. This technique has considerable cosmetic effects, but it cannot solve the problems (causes) of the pathology itself. It may recur after sclerotherapy. The contraindications for this intervention are pregnancy, breastfeeding and intolerance to the ingredients of the drug.
- Peel off. Using this method, the thinnest probe is used to remove the diseased vein. The feature of surgery is that only the diseased part of the blood vessel can be removed, leaving the healthy part. The operation is performed by two endoscopic punctures located on either side of the inflamed blood vessel. In other words, the scars and scars after this intervention will not be visible.
- Veinectomy. Diseased veins can also be removed through several small incisions in the skin.
- Laser coagulation. Irradiate the lumen of the diseased blood vessel with a laser. As a result, the venous cavity is completely overgrowth.
Mature surgery (abdominal surgery) is called phlebectomy. Using this method, the surgeon will make a complete incision in the skin of the leg to remove the entire superficial vein. The signs of this operation are:
- A large number of varicose veins;
- The large cavity (cavity) of the diseased blood vessel (more than 10 mm);
- Thrombophlebitis;
- The presence of large varicose veins;
- The formation of the patient's trophic ulcer;
- Minimally invasive surgery is not effective.
Traditional treatment
In the initial stages of pathology, you can also turn to folk methods for the treatment of varicose veins. Especially in combination with medical treatment, the following folk remedies can be used:
- Tomatoes are green. Place the vegetable slices on the inflamed vein area and secure with a bandage. You need to change such applications every 2-3 hours. The course of treatment until the condition is significantly improved.
- potato. Put a bandage soaked in freshly squeezed potato juice on your leg. Cover the top with plastic wrap. This application is best done at night until the patient's condition improves.
- Apple cider vinegar. It is best to be homemade. The vinegar is diluted with water (1 cup of water and 2-3 tablespoons of vinegar). The bandage is moistened in the solution and applied to the diseased vein area. The bandage is fixed at night. You can also use this solution at night to simply lubricate your feet. It is shown to take vinegar water and internally. Add 1 tablespoon of apple cider vinegar and a teaspoon of honey to a glass of water to prevent the vinegar from burning the esophagus (the wall of the esophagus is easily affected by acid). Drink the mixture on an empty stomach in the morning. The course of vinegar treatment is 30 days.
- Horse chestnut. The flower volume of the plant is 50 grams. Pour 0. 5 liters of alcohol and keep it in a dark place for two weeks, shaking the mixture regularly. The finished product is filtered through a sieve and consumed 3 times during the day, one tablespoon at a time. The mixture was washed with water. The course of treatment is 7 days. Then there was a 14-day break, and then another 7-day course. According to this plan, treatment is carried out until the end of the infusion. The treatment plan can then be prepared again and repeated.
- Burdock. In this case, use the fresh leaves of the plant to eliminate the disease. At night, Vishnevsky’s ointment was applied to the sore feet, and a piece of burdock leaf. Everyone was secured with bandages and put on compression stockings. The bandage was worn for three days, and then removed, everything was washed away. It can be treated in this way all summer, while fresh burdock grows.
important:This treatment is contraindicated for patients with high gastric acidity.

in conclusion
It is worth noting that varicose veins are an irreversible pathology in most cases. Therefore, it is very important to take good care of the health of the feet. Especially if there is a genetic predisposition for varicose veins. Give up bad habits, keep your daily diet balanced, walk more every day, and drink enough clean water is enough. When the slightest signs of varicose veins appear, it is recommended to contact a qualified phlebologist immediately to prevent complications of the disease. Remember, your health and the internal health of your feet are entirely up to you. The hands of modern medicine and professionals can do miracles.























